Lewy Body Dementia (LBD) impacts millions of families across the world. Yet many people are still unfamiliar with its progressive nature and distinctive symptoms. Lewy Body Dementia has seven stages that patients, caregivers and families need to be aware of when facing this difficult disease. Unlike other forms of dementia, LBD has its own characteristics which set it apart from other types and stages of dementia, such as Alzheimer’s disease and vascular dementia and 7 Stages Of Frontotemporal Dementia. Early recognition and accurate staging, however, is critical in effective care planning.
This guide takes a closer look at each stage of Lewy Body Dementia progression. It helps you to identify symptoms, understand treatment options, and plan for the future. Whether you are newly diagnosed or worry about cognitive changes in your loved one, this overview provides some great insights into how to deal with this complex neurological condition.
Understanding What Lewy Body Dementia is?
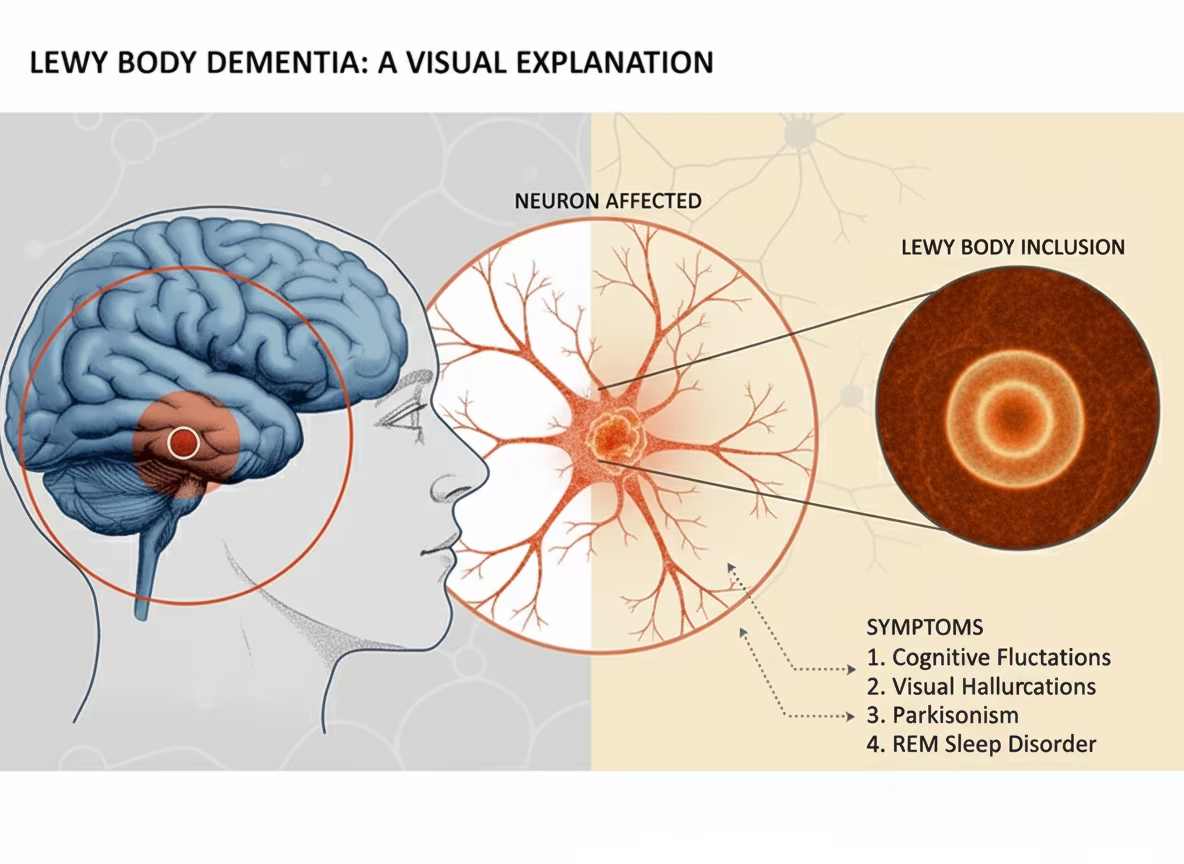
Lewy Body Dementia is the second most common form of progressive dementia after Alzheimer’s disease. It is caused by abnormal protein deposits called Lewy bodies which accumulate in brain cells and affect normal brain function. Unlike other types of dementia, LBD directly impacts multiple brain systems simultaneously, resulting in a combination of cognitive, movement and behavioral problems.
People often ask, “Is dementia hereditary?” when a family member is diagnosed with LBD. Although in some cases there may be a genetic component, most cases of LBD are sporadic and not inherited. A family history of dementia, however, can increase your risk slightly.
LBD is distinguished by its classic triad: waxing and waning cognition, visual hallucinations and Parkinsonism. Symptoms may occur in combination and to different degrees, making the 7-stage model for Lewy Body Dementia useful to evaluate disease progression and for planning care.
Expert Insight: ” Lewy Body Dementia is one of the most difficult conditions to diagnose in neurology. Its symptoms are variable, so a patient might be totally normal one day and severely impaired the next. It is crucial to recognize this pattern early in order to provide an accurate diagnosis and treatment plan. – Dr. Sarah Chen, Director of Movement Disorders, Johns Hopkins Medical Center
7 Stages of Lewy Body Dementia
Stage 1: No Cognitive Decline (Preclinical Phase)
In the earliest stage, people appear and behave normally, with no obvious memory or thinking problems. Tiny changes in the brain may be starting but haven’t caused symptoms yet. This stage can persist for years; and many people never progress further than this. Family members should be aware of this stage’s existence, especially if they are considering getting genetic counseling and learning about the risk of dementia.
During this preclinical phase, maintaining mental and physical activity, with regular exercise, social activity, and activities that exercise the brain, may delay or prevent the transition to stages of symptoms.
Stage 2: Very Mild Cognitive Decline (Age-Related Changes)
During the second stage people may have minor, normal-age-related changes. They may not remember where a key was left or have trouble remembering a familiar name. The changes are typically so mild that they don’t interfere with daily life and independence.
Contrary to amnesia vs dementia, where amnesia is characterized by distinct episodes of memory loss, this stage is characterized by general, slow cognitive decline. Family members might see a slight change in personality or an increase in anxiety in new situations, but these are signs that can be easily missed as the early symptoms of dementia.
Stage 3: Mild Cognitive Decline (Early Confusional Stage)
Stage 3 is the beginning of apparent cognitive changes beyond those of normal aging. The seven stages of Lewy Body Dementia become more apparent as a person begins to have trouble with complex tasks, problem solving and planning.
The symptoms during this phase are:
- Finding it difficult to concentrate for long periods
- Decreased ability to work or be in social situations
- problems understanding written material and remembering information
- Increasing concern about one’s memory or thinking skills.
- Fluctuating Attention and Alertness
Visual hallucinations may begin at this stage, often in the form of realistic images of animals or people that are not actually present. These hallucinations tend to be very well formed and detailed, unlike the fragmentary ones associated with other conditions.
Stage 4: Moderate Cognitive Decline (Late Confusional Stage)
The fourth stage is a significant milestone in the seven-stage progression of Lewy body Dementia. At this stage, patients start requiring assistance with complex daily tasks, but can still care for themselves with basic personal care.
Notable changes include:
- Difficulty managing finances and paying bills
- Problems with cooking complex meals
- Confusion about time and place
- Social withdrawal, because of embarrassment about symptoms
- More frequent and intense visual hallucinations
- Beginnings of movement difficulties that are similar to Parkinson’s disease
The Lewy Body Dementia ICD-10 classification (G31.83) usually takes place from this stage onwards, as the symptoms were clinically significant and diagnosable. Standard assessment tools are commonly utilized during this phase in order to determine baseline functioning and monitor change over time.
Stage 5: Moderately Severe Cognitive Decline (Early Dementia Stage)
Stage 5 is the transition to more serious cognitive impairment that must be supported by daily assistance. In this phase, the progression of Lewy Body Dementia speeds up, involving several areas of symptoms simultaneously.
Some characteristic features are:
- Notable gaps in memory involving recent as well as distant events
- Difficulty choosing appropriate clothing for the weather or the occasion
- Need for help with personal hygiene and grooming
- Increasing confusion about one’s identity and history
- Severe sleep problems, such as REM sleep behavior disorder
- Pronounced movement problems, which affect walking and coordination
The connection between muscle loss and dementia becomes more evident as people become less physically active, which causes muscle weakness and leads to greater risk for falls. This stage typically involves safety and can lead to the need to consider care facility options.
Stage 6: Severe Cognitive Decline (Middle Dementia Stage)
The sixth stage of the disease is severe cognitive impairment affecting nearly all areas of daily functioning. Understanding the 7 stages of Lewy Body Dementia is a crucial part of the care decisions made by family members during this difficult time.
Major symptoms include:
- Extensive memory loss that includes the recognition of close family members
- Significant personality changes and behavioral problems
- Loss of awareness of recent events and surroundings
- Needs a great deal of help with basic activities of daily living
- Increased susceptibility to infections and other health problems
- Severe movement difficulties and need of mobility aids or help
The Fast Scale Dementia assessment tool is particularly helpful during this stage of assessment to determine functional capabilities and predict care needs. Healthcare professionals use this staging system along with other tests to make treatment choices.
Stage 7: Very Severe Cognitive Decline (Late Dementia Stage)
The final stage of the seven stages of Lewy Body Dementia is characterized by severe mental and physical decline. People often cannot communicate, identify loved ones or care for themselves.
End‑stage signs include:
- limited or no verbal communication
- Unable to walk without significant assistance
- loss of bowel and bladder control
- Difficulty swallowing, which can cause a risk for nutrition and hydration
- Increased risk of infection, particularly pneumonia
- Needs to be under constant care and supervision
This stage can rapidly progress to a stage of decline as a result of complications or other medical conditions. Palliative care methods have become more and more important for comfort and dignity.
Lewy Body Dementia vs Other Dementias
Understanding the differences between LBD and other forms of dementia helps to understand the unique way it progresses over the seven stages. While Alzheimer’s disease primarily attacks memory first, LBD attacks several different brain systems simultaneously from the beginning.
Some distinguishing characteristics are:
- Fluctuating cognition: Unlike Alzheimer’s, which is steady decline, LBD patients have bad days and good days. Cognitive performance may vary from hour to hour or day to day.
- Visual hallucinations: Detailed hallucinations occur early in LBD. They usually depict people or animals and rarely are threatening.
- Movement disorders: Parkinson-like symptoms including tremor, stiffness and slowness occur in many LBD patients, sometimes even before the onset of cognitive changes.
- Sleep Disturbances: REM sleep behavior disorder, a condition in which people act out their dreams physically, is present in up to 80% of patients with LBD, sometimes preceding other symptoms by years.
Clinical perspective: “Successfully managing Lewy Body Dementia begins with the fact that it is not just a memory disorder – it is a multi-system disorder.” We have to treat cognition, movement, sleep, and behaviour together, for the best results.” “People with LBD should have additional testing to determine if they have other conditions that can be treated, which may improve their symptoms.” – Dr. Michael Rodriguez, Neurologist and LBD Specialist, Mayo Clinic
Treatment Approaches Across the 7 Stages
Treatment strategies for Lewy Body Dementia must address the complex symptom profile and take into consideration the progressive nature evidenced in the 7 stages of Lewy Body Dementia. No cure currently exists but different interventions can help manage the symptoms and improve the quality of life.
Medication Management
- Cholinesterase Inhibitors – Drugs such as rivastigmine and donepezil are helpful in the cognitive symptoms and may work better in LBD than other dementias. These medications work best during stages 3-5 of the progression.
- Antipsychotic Medications – Traditional antipsychotics can be dangerous for LBD patients because of severe sensitivity reactions. When hallucinations become problematic then alternative approaches or carefully selected medications must be considered.
- Movement Disorder Treatment – Carbidopa – levodopa may help with Parkinson symptoms but require careful monitoring as it may make the symptoms of hallucinations and confusion worse.
- Sleep Medications – Melatonin and other sleep aids can help to address the severe sleep disturbances that are common throughout the 7 stages of Lewy Body Dementia.
Non-Pharmacological Interventions
- Physical Therapy – Maintaining mobility and preventing falls becomes increasingly important as the person moves through the stages. Routine physical therapy can help maintain function and decrease the risk of falling.
- Occupational Therapy – Adapting the home environment and daily routines can ensure independence for a longer time while conducting safe activities throughout disease progression.
- Speech Therapy – Communication strategies and swallowing evaluation become key at later stages in order to avoid complications and maintain quality of life.
- Cognitive Stimulation – Stimulating activities, based on current cognitive abilities, can help maintain mental functioning and offer meaningful experiences through all stages.
Treatment Cost Considerations
Understanding the financial aspects of LBD care helps families plan appropriately during the 7 stages of Lewy Body Dementia:
Medication Costs (Monthly):
- Cholinesterase inhibitors: $200-$400 (not covered by insurance)
- Levodopa/carbidopa: $50 – $150 (for generic versions)
- Sleeping pills: $30 – $200 (depending on type)
- Antipsychotic alternatives: $300 — $800 for newer formulations
Professional Care Services:
- Neurologist consultations: $300 — $600 for each visit
- Physical therapy: $100 to $200 per session
- Occupational therapy $120 – $250 per session
- Speech therapy: $100‑$200 per session
- Home health Aid: $20‑$30 per hour
- Adult day care: $50‑$100 per day
Long-term Care Options:
- Assisted living facilities: $3,000- $6,000 per month
- Memory care units: $4,000‑$8,000 per month
- Skilled nursing facilities: $5000 – $10,000 per month
- In‑home care (24/7): $15,000‑$25,000 per month
Note: Costs vary significantly by geographic location and insurance coverage. Medicare and Medicaid may cover certain services.
Managing Behavioral and Psychological Symptoms
Each of the 7 stages of Lewy Body Dementia presents its own set of behavioral challenges that need to be approached in specific ways. Learning about these patterns will allow families and caregivers to learn coping skills.
Early-Stage Interventions (Stages 1-3)
In the early stages, it’s important to stick to routines, alleviate stress and offer emotional support. Minimal environmental changes can be used to manage minor confusion and anxiety and maintain independence.
Middle Stage Management (Stages 4-5)
As the symptoms become more severe, it is important that you have structured daily routines. Managing hallucinations involves the balance between validation and reality orientation — no confrontation, but make sure safety is maintained.
Advanced Stage Care (Stages 6-7)
Late-stages care focuses on comfort, dignity and support for the family members. Behavioral symptoms can decrease as the cognitive decline develops, but the demand for hands-on physical care increases.
Family Support and Caregiver Resources
The 7 stages of Lewy Body Dementia impact not only people diagnosed with it, but entire families. Stress, emotional strain, and practical difficulties increase as the disease progresses.
Educational Resources
Learning about disease progression can help families plan for the future and plan for the future of their care. Support groups for LBD specifically are a great way to gain valuable connections with others on similar journeys.
Respite Care Services
Regular breaks from the caring role helps to prevent burnout and maintain caregiver health throughout the length of the symptoms.
Advanced Care Planning
Early discussions about future care preferences, legal documents and end-of-life wishes should occur when individuals are still able to have a meaningful contribution to these important decisions.
Research and Future Directions
Current research into Lewy Body Dementia focuses on understanding the mechanisms of the disease, developing improved diagnostic tools and creating more effective treatments. Studies that examine 7 stages of the disease help researchers identify points for intervention and treatment effectiveness.
Promising areas of research are:
- Biomarker development to allow earlier diagnosis
- Neuroprotective treatments (to slow progression)
- Gene Therapy in Familial cases
- Better ways to manage symptoms
Clinical trials continue investigating new medications and non-pharmacological interventions that might alter disease progression or improve quality of life across all stages.
Recent Research Developments (2023-2025):
- Biomarker Studies: New cerebrospinal fluid and blood tests showing promise for earlier LBD detection (Journal of Neurochemistry, 2024)
- Digital Therapeutics: Virtual reality cognitive training showing 23% improvement in attention scores during stages 3-4 (Frontiers in Aging Neuroscience, 2024)
- Precision Medicine: Genetic profiling helping predict medication responses and optimize treatment plans (Nature Medicine, 2023)
- Sleep Intervention Trials: Targeted REM sleep treatments reducing hallucination frequency by 35% (Sleep Medicine Reviews, 2024)
- Neuroprotective Compounds: Phase II trials of antioxidant therapies showing promise in slowing progression (Lancet Neurology, 2023)
Research Perspective: “We are now in an exciting time for Lewy Body Dementia research. The combination of biomarker discovery, digital health tools and precision medicine are opening up new possibilities for earlier diagnosis and more targeted interventions. – Dr. Jennifer Walsh, Ph.D., MD, FACAP, LBD Research Initiative Lead Researcher, National Institute on Aging
When to Seek Professional Help
Knowing when to get medical attention is essential in all seven stages of Lewy Body Dementia. Early consulting will ensure an accurate diagnosis, a personalized treatment plan and access to the necessary resources.
Symptoms that need urgent medical care include:
- Sudden changes in the level of thinking or behavior
- Developing or increasing problems with movement
- Serious medication reactions/side effects
- Safety issues about driving, cooking, or other day-to-day activities
- Signs of depression, anxiety or other psychiatric symptoms
Regular medical monitoring is done to track the disease progression and makes it possible to timely adjust treatments at each stage.
Stage-by-Stage Care Checklists
Understanding the 7 stages of Lewy Body Dementia becomes more actionable with specific checklists for each phase.
Stages 1-2 Preparation Checklist
Early Planning Actions:
- [ ] Develop baseline measurements of cognitive and physical function
- [ ] Make advance cares and other legal papers
- [ ] Find local neurologists and movement disorder experts
- [ ] Join LBD Support Groups and Education Programs
- [ ] Write down your skills and your personal preferences.
- [ ] Review insurance coverage for future healthcare needs
- [ ] Add safety features, such as bars and better lighting
- [ ] Assemble emergency contact lists & medical information packet
Stages 3-4 Management Checklist
Active Symptom Management:
- [ ] Schedule regular medication reviews with neurologist
- [ ] Create a daily schedule and follow visual schedules.
- [ ] Work on driving safety issues and alternatives
- [ ] Arrange home safety evaluation by occupational therapist
- [ ] Identify a physical therapist and speech language pathologist.
- [ ] Create calm, familiar environments to reduce confusion
- [ ] Implement strategies to deal with hallucinations
- [ ] Consider adult day programs for social engagement
- [ ] Review financial management and bill paying support
- [ ] Update emergency medical information & contacts
Stages 5-7 Advanced Care Checklist
Comprehensive Support Planning:
- [ ] Evaluate residential care and wait lists
- [ ] Arrange for mobility aids and home modifications
- [ ] Develop palliative care team relationships
- [ ] Develop Comfort Oriented Daily Routines
- [ ] Arrange for respite care for primary caregivers
- [ ] Review end-of-life preferences and documentation
- [ ] Coordinate with a number of healthcare specialists
- [ ] Develop fall prevention and safety measures
- [ ] Respond to nutrition and swallowing issues
- [ ] Plan for 24/7 care needs as well as staffing
Conclusion
Lewy Body Dementia has seven stages which describe how the disease can progress. But everyone’s journey is a unique one. Some move quickly from one stage to the next. Others change slowly over the course of many years. Knowing the stages is helpful in making informed decisions about your care and making plans. If you are living with LBD or caring for a loved one, keep the needs of the present in mind, be flexible and contact doctors, family, and community services. With Right care, individuals can maintain the quality of life and meaningful connections at every stage.
Facing Lewy Body Dementia? Knowing these 7 stages can inform your care planning and decision making. Whether you are living with LBD or caring for someone else, remain flexible, focus on the present and rely on medical and community resources that can empower and support you through the journey.
Frequently Asked Questions
1. How quickly do people progress through the 7 stages of LBD?
Lewy Body Dementia does not progress in the same way in every patient. Some people remain relatively stable for several years, whereas others do have a fast decline. On average, the disease progresses over approximately 5 to 8 years but can actually last anywhere from 2 to 20 years, depending on the person’s overall health, level of care and other individual factors.
2. Is dementia hereditary, specifically Lewy Body Dementia?
Many people are concerned about hereditary dementia. In most cases of Lewy Body Dementia, it is not genetically passed down, although this does have a small influence. If there is a family history of dementia or Parkinson’s disease, then the risk is likely to be higher. Genetic counseling may be of assistance to families with multiple affected members.
3. Can someone skip stages in the 7 stages of Lewy Body Dementia progression?
Yes, the 7 stages are merely a guideline. Because LBD is sometimes fluctuating, a person may skip stages, or may stop at one stage, or may exhibit symptoms from more than one stage at a time.
4. What’s the difference between amnesia vs dementia in LBD patients?
Amnesia is the specific loss of memory due to a specific injury. Dementia in the case of LBD is a gradual decline in thinking, which includes memory loss, movement problems, hallucinations and sleep disturbances.
5. How does the Fast Scale Dementia assessment relate to LBD staging?
The FAST scale Functional Assessment Staging Tool is used to assess the daily function in Lewy Body Dementia in the later stages. It complements a 7-stage system that focuses on specific symptoms. Together, these tools give healthcare providers a clearer picture of disease progression and help them to monitor decline and plan effective care.
6. What role does muscle loss play in dementia progression?
Muscle waste in LBD is due to decreased physical activity and altered nervous system. Physical therapy can maintain strength and function with the progress of the disease.
7. When should families start planning for advanced stages?
Families need to begin planning early – ideally in stages 1 to 3 – so that legal, financial and care preferences can be addressed whilst the person is still able to make contributions to decisions.
8. Can treatments slow progression through the 7 stages?
There is no treatment available that stops the progression of Lewy body dementia (LBD). However, the use of cholinesterase inhibitors, physical therapy and cognitive stimulation can help slow the decline and enhance quality of life. With treatment usually occurring early, outcomes are better.










1 thought on “Lewy Body Dementia: Stages, Symptoms & Complete Treatment”